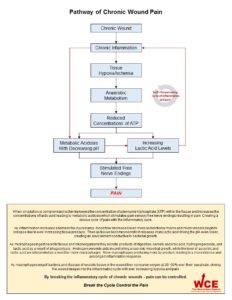
Pain is a frequent symptom of patients living with chronic wounds and contributes to suffering and reduced quality of life.9,65,66 Studies have shown that more than 80% of patients with chronic wounds are in constant pain and half of them classify their pain as moderate to severe.1-4 Pain is subjective and can best be described as whatever the patient says it is and exists whenever they says it does.67 In a large prospective study of 758 patients it was found that the more chronic the duration, the higher the reported wound pain (P = 0.022).5 This study also reiterates the importance of early and aggressive pain treatments to avoid the potential spiraling effect of chronic wound pain later on.5,64 In recent years, there has been an increasing awareness of the amount of pain patients with chronic wounds experience.6,7,12 Researchers in 2002 conducted a multinational survey of over thirty-nine thousand wound care practitioners from eleven different countries and found they rated dressing removal as the time of greatest pain.12 Although only limited research has been completed on chronic wound pain, it’s not surprising that most has focused on pain at dressing removal. 6-11 One consistent point stands out in these papers: an agreement that the underlying cause of chronic wound pain is related to inflammation.6,7,11 Despite this, an extensive literature search could not find a clinical pathway for chronic wound pain related to chronic wound inflammation. The purpose of this paper is to present such a pathway and demonstrate that by breaking the chronic wound inflammation cycle, wound pain can be better controlled. Following tissue injury, persistent inflammation triggers a cascade of events that activates local pain receptors. This results in greater sensitivity of the surrounding skin and deeper structures in the wound base. The pain itself can be caused by tissue damage (nociceptive) or nerve damage (neuropathic). The molecular environment of chronic wounds contains elevated levels of inflammatory cytokines and proteases, with low levels of mitogenic activity, and cells that are approaching senescent which fail to respond to growth factors.13,24 Although the inflammatory profile differs in the various types of chronic wounds, this general relationship affects all chronic wounds.13,24,25 When the inflammatory cycle is prolonged, a “vicious cycle” characteristic of all chronic wounds, is created.13 This “vicious cycle” was first describe by Mast and Schultz in 1996 and clearly explain the self-sustaining nature of a prolonged inflammatory phase and its far reaching effects. Their diagrammatic representation of the pathophysiologic characteristic of acute and chronic wounds is an excellent representation of the micro wound environment to date and has been validated by many other researchers.24,25,26,27,28,29,30,31,32,33,34,35 Once the chronic wound becomes stuck in the inflammatory phase and wound healing is prolonged, pain increases5. As the same chronic wound begins to heal, the micro-wound environment shifts to one that resembles a healing wound and wound pain is reduced; the connection between prolonged inflammation and pain seems clear.5-7,11 Edema remains one of the body’s first responses to inflammation. Chronic edema causes peri-capillary cuffing which starves tissue by reducing the amount of oxygen and nutrients delivered to the wound tissue.39,40 The presence of infection only widens this oxygen debt.41 This hypoxic environment helps to drive the wound deeper into a “vicious cycle” of self perpetuating inflammation as describe by Mast and Schultz.13 Untreated, overtime edema contributes to a shift from hypoxic to ischemic, as fibrin is deposited around the capillary beds forming a fibrin cuff. As capillary beds begin to collapse because of excessive tissue pressure, blood flow becomes sluggish and leukocytes begin to adhere to each other resulting in “plugging” of the capillaries.42,43,44 This results in an ischemic-reperfusion injury.45-56 The lack of available oxygen leads to anaerobic metabolism which reduces concentrations of adenosine triphosphate (ATP) and results in metabolic acidosis. The reduction of ATP facilitates increased lactate with decreasing pH. This “excites” nociceptors and produces activation of pH-sensitive ion channels, resulting in pain.14 Likewise, if there is sufficient oxygen for aerobic metabolism, then the by-product acid is metabolized into carbon monoxide and water, representing the final step of complete metabolism. As a result, pain is reduced or alleviated.15 – 22 This theory may explain why acute wounds have lower levels of associated pain when compared to chronic wounds. It also explains the success Coloplast is having with its ibuprofen-foam in reducing wound pain, as ibuprofen is a non-steroidal anti-inflammatory drug (NSAID).57-62 In 2009 a team of researchers clearly demonstrated that ibuprofen could down regulate proinflammatory cytokines when applied topically, further supporting this theory.63 This theory has also been indirectly supported by researchers using transcutaneous oxygen tensions measurement (TcPO2), who have demonstrated that edema reduces TcPO2 levels: once edema is controlled these levels increase.36,37,38 By breaking the inflammatory phase of healing, chronic wound pain can be controlled.
References
- Gottrup et al. Reducing wound pain in venous leg ulcers with Biatain Ibu: A randomized, controlled double-blind clinical investigation on the performance and safety. Wound Repair and Regeneration 2008; 16: 616-626.
- Woo et al. Assessment and management of persistent (chronic) and total wound pain. International Wound Journal 2008; 5(2): 205-215.
- Pieper et al. Pain associated with venous ulcers in injecting drug users. Ostomy Wound Management 1998; 44: 54–67.
- Nemeth et al. Understanding venous leg ulcer pain: results of a longitudinal study. Ostomy Wound Management 2004; 50: 34–36.
- Franks et al. Do clinical and social factors predict quality of life in leg ulcerations. International Journal of Lower Extremity Wounds. 2006; 5: 236-243.
- European Wound Management Association. Pain at Wound Dressing Changes. London, UK: Medical Education Partnerships LTD, 2002.
- World Union of Wound Healing Societies. Principles of Best Practice: Minimising Pain at Wound Dressing-Related Procedures: A Consensus Document. London, UK: Medical Education Partnerships LTD, 2004.
- Woo et al. Assessment and management of persistent (chronic) and total wound pain. International Wound Journal. 2008; 5 (2): 205-214.
- Acton C. The holistic management of chronic wound pain. Wounds UK. 2007; 3 (1): 61-69.
- Woo. et al. Chronic wound pain: a conceptual model. Skin and Wound Care. 2008; 21 (4): 175-190.
- Krasner D. Pain management. In: Falabella AF, Kirsner RS. (Eds) Wound Healing. Boca Raton: Taylor & Francis. 2005.
- Moffatt. Et al. Understanding wound pain and trauma: an international perspective. In: Pain at Wound Dressing Changes. London, UK: Medical Education Partnerships LTD, 2002: 2-7.
- Mast BE, Schultz GS. Interactions of cytokines, growth factors, and proteases in acute and chronic wound. Wound Repair and Regeneration. 1996; 4: 411-420.
- Yeoh-Ellerton S, Stacey MC. Iron and 8-isoprostance levels in acute and chronic wounds. Journal for Investigative Dermatology. 2003; 121: 918-925.
- Kim TJ, Freml L, Park SS, Brennan TJ. Lactate concentrations in incisions indicate ischemic-like conditions may contribute to postoperative pain. The Journal of Pain. 2007; 8 (1): 59-66.
- Sutherland SP, Cook SP, McCleskey EW. Chemical mediators of pain due to tissue damage and ischemia. Progress in Brain Research. 2000; 129: 21-38.
- Woo YC, Park SS, Subieta AR, Brennan TJ. Changes in tissue pH and temperature after incision indicate acidosis may contribute to postoperative pain. Anesthesiology. 2004; 101: 468-475.
- Reeh PW, Steen KH. Chapter 8. Tissue acidosis in nociception and pain. Progress in Brain Research. 1996; 113: 143-151.
- Steen KH, Reeh PW. Sustained graded pain and hyperalgesia from harmless experimental tissue acidosis in human skin. Neuroscience Letters. 1993; 154 (1-2): 113-116.
- Issberner U, Steen KH, Reeh PW. Pain due to tissue acidosis: a mechanism for inflammatory and ischemic myalgia? Neuroscience Letters. 1996; 208 (3): 191-116.
- Birklein F, Weber M, Neundörfer B. Increased skin lactate in complex regional pain syndrome: evidence for tissue hypoxia? Neurology. 2000; 55: 1213-1215.
- Naves LA, McCleskey EW. An acid-sensing ion channel that detects ischemic pain. Brazilian Journal of Medical and Biological Research. 2005; 38 (11): 1561-1569.
- Koban M, Leis S, Schultze-Mosgau S, Birklein Tissue hypoxia in complex regional pain syndrome. Pain 2003; 104 (1): 149-157.
- Tarnuzzer R, Schultz G. Biochemical analysis of acute and chronic wound environments. Wound Repair and Regeneration. 1996; 4 (3): 321-325.
- Nwomeh B, Yager D, et al. Physiology of the chronic wound. Clinics Plastic Surgery. 1998; 25: 341-356.
- Schultz G, Mast B. Molecular analysis of the environment of healing and chronic wounds: cytokines, proteases, and growth factors. Wounds. 10 (suppl F): 1F, 1998.
- Schultz GS. Molecular regulation of wound healing. In: Bryant RA and Nix DP, ed. Acute and Chronic Wounds: Current Management Concepts. 3rd Philadelphia: Mosby, 2007: 82-99.
- Goldman R. Growth factors and chronic wound healing: past, present, and future. Advances in Skin and Wound Care. 2004; 17 (1): 24-35.
- Berg Vande J, Robson M. Arresting cell cycles and the effect on wound healing. Surgical Clinics of North America. 2003; 83: 509-520.
- Henry G, Garner W. Inflammatory mediators in wound healing. Surgical Clinics of North America. 2003; 83: 483-507.
- Staiano-Coico L, et al. Wound fluid: a reflection of the state of healing. Ostomy Wound Management. 2000; S46 (1A): 85-93.
- Yager D, Nwomeh B. The proteolytic environment of chronic wounds. Wound Repair and Regeneration. 1999; 7: 433-356.
- Trengrove N, Stacey M, et al. Analysis of the acute and chronic wound environment: the role of proteases and their inhibitors. Wound Repair and Regeneration. 1999; 7: 442-452.
- Trengrove N, Bielefeldt-Ohmann H, et al. Mitogenic activity and cytokine levels in non-healing and healing chronic leg ulcers. Wound Repair and Regeneration. 2000; 8: 13-25.
- Bucalo B, Eaglstein W, et al. Inhibition of cell proliferation by chronic wound fluid. Wound Repair and Regeneration. 1993; 1: 181-186.
- Ballard J, Eke C, et al. A prospective evaluation of transcutaneous oxygen measurements in the management of diabetic foot problems. Journal of Vascular Surgery. 1995; 22 (4): 485-492.
- Byren P, Provan J, et al. The use of transcutaneous oxygen tension measurements in the diagnosis of peripheral vascular insufficiency. Annals of Surgery. 1984; 200 (20): 159-165.
- Hanna G, Fujise K, et al. Infrapopliteal transcatheter interventions for limb salvage in diabetic patients: importance of aggressive interventional approach and role of transcutaneous oximetry. Journal of the American College Cardiology. 1997; 30: 664-669.
- Burn K, Whimster I, et al. Pericapillary fibrin in the ulcer-bearing skin of the leg: the cause of lipodermatosclerosis and venous ulcerations. British Medical Journal. 1982; 285: 1693-1695.
- Browse N, Burnand K. The cause of venous ulcerations. Lancet. 1982; 28 (292): 243-245.
- Rabkin J, Hunt T. Infection and oxygen. In: Jefferson CD and Hunt TK, ed. Problem Wounds: The Role of Oxygen. New York: Elsevier, 1988: 1-16.
- Smith P. The microcirculation in venous hypertension. Cardiovascular Research. 1996; 32 (4): 789-795.
- Van de Scheur M, Falanga V. Pericapillary fibrin cuffs in venous disease. Dermatologic Surgery. 1997; 233: 955-959.
- Kalra M, Gloviczki P. Surgical treatment of venous ulcers: role of subfascial endoscopic perforator vein ligation. Surgical Clinics of North America. 2003; 22 (3): 671-705.
- Greenwood JE, Edwards AT, McCollum CN. The possible role of ischaemia-reperfusion in the pathogenesis of chronic venous ulceration. Wounds. 1995; 7: 211-219.
- Coleridge Smith PD. The microcirculation in venous hypertension. Cardiovascr Res 1996; 32: 789-795.
- Coleridge Smith PD. Oxygen, oxygen free radicals and reperfusion injury. Wounds.1996; 8: 9-15.
- Coleridge Smith PD. Neutrophil activation and mediators of inflammation in chronic venous insufficiency. J Vas Res. 1999; 36: 24-36.
- Kilgore KS, Todd III RF, Lucchesi BR. Reperfusion injury. In: Gallin JI, Snyderman R, editors. Inflammation: basic principles and clinical correlation. Lippincott, Williams & Wilkins, 1999: 1047-1060.
- Nixon J. The pathophysiology and etiology of pressure ulcers. In: Morrison M, editor. The prevention and treatment of pressure ulcers. Edinburgh: Mosby, 2001: 17-36.
- Fagrell B, Jorneskog G, Intaglietta M. Disturbed microvascular reactivity and shunting – a major cause for diabetic complications. Vasc Med 1999; 4: 125-127.
- Dinh TL, Veves A. Microcirculation of the diabetic foot. Curr Pharm Des 2005; 11: 2301-2309.
- Dinh TL, Veves A. A review of the mechanisms implicated in the pathogenesis of the diabetic foot. Int J Low Exterm Wounds 2005; 4: 154-159.
- Tooke JE, Brash PD. Microvascular aspects of diabetic foot disease. Disease. Diabet Med. 1996; 13 (Supp. 1): S26-S29.
- Mustoe TA, O’Shaughnessy K, Kloeters O. Chronic wound pathogenesis and current treatment strategies. Plastic and Reconstructive Surgery. 2006; 117; 7S: 35S-41S.
- Menke NB, Ward KR, Tarynn M, Bonchey DG, Diegelmann RF. Impaired wound healing. Clinics in Dermatology. 2007; 25 (1): 19-25.
- Sibbald RG, Coutts P, Fierheller M, Woo K. A pilot (real-life) randomized clinical evaluation of a pain-relieving foam dressing: (ibuprofen-foam versus local best practice). International Wound Journal. 2007; 4 (suppl. 1): 16-23.
- Gottrup F, Jørgensen B, Karlsmark T, Sibbald RG, et al. Less pain with Biatain-Ibu: initial findings from a randomized, controlled, double-blind clinical investigation on painful venous leg ulcers. International Wound Journal. 2007; 4 (suppl. 1): 24- 34.
- Jørgensen B, Friis G, Gottrup F. Pain and quality of life for patients with venous leg ulcers: proof of concept of the efficacy of Biatain – Ibu, a new pain reducing wound dressing. Wound Repair and Regeneration. 2006; 14 (3 ):233-239
- Flanagan M, Vogensen H, Haase L. Case series investigating the experience of pain in patients with chronic venous leg ulcers treated with a foam dressing releasing ibuprofen. World Wide Wounds. worldwidewounds.com/2006/april/Flanagan/Ibuprofen-Foam-Dressing.html
- Gad P, Shewale S, Drewes AM, Arendt-Nielsen, L. Effect of a local ibuprofen dressing on healing of experimentally induced laser wounds. In: Gottrup F, et al. (Ed.) European Wound Management Association Conference; 2006 May 17-20; Prague. Frederiksberg: Congress Consulting.
- Romanelli M, Dini V, Polignano R, Maggio G. Ibuprofen slow-release foam dressing reduces wound pain in painful exuding wounds: Preliminary findings from an international real-life study. Journal of Dermatological Treatment. 2009; 20 (1): 19-26.
- Redpath M, Marques CMG, Dibden C, et al. Ibuprofen and hydrogel-released ibuprofen in the reduction of inflammation-induced migration in melanoma cells. British Journal of Dermatology. 2009; 161 (1): 25-33.
- American Academy of Pain Medicine. The necessity for early evaluation and treatment of chronic pain patient. A Consensus Statement. Glenview, IL: AAPM, 1997. Available from URL: http://www.painmed.org.
- Franks P, Moffatt C. Community leg ulcer clinics: effects on quality of life. Phlebology. 1994; 9: 83-86.
- Price P, Harding K. Measuring health-related quality of life in patients with chronic leg ulcers. Wounds. 1996; 8 (3): 91-94.
- McCaffery M. Nursing management of the patient with pain. Philadelphia, 1972, JB Lippincott.